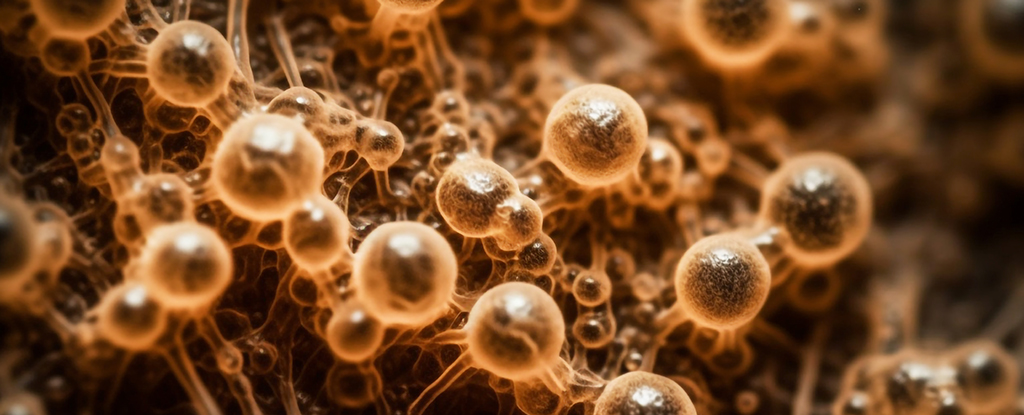
Cases of the fungal infection Candida auris are rising rapidly and coming from more sources too, a new US study reveals.
C. auris was first reported in the US in 2016 and is considered an “urgent antimicrobial resistance threat” in hospitals, according to the Centers for Disease Control and Prevention (CDC).
Focusing on a large health system in Miami, Florida, the new research found that reported clinical cases had risen from 5 in 2019 to 115 in 2023 – a considerable jump of 2,200 percent in four years.
“Consistent with US national trends, C. auris rapidly spread in our community as noted by a sharp increase in the identification of C. auris from clinical cultures in 2020 and 2021, followed by a less steep rise in 2022 and 2023,” writes the US team in their published paper.
Many strains of C. auris don’t respond to regular treatments, and are resistant to common cleaners and disinfectants too. The fungus spreads quickly in hospitals, often via equipment like catheters and breathing and feeding tubes.
frameborder=”0″ allow=”accelerometer; autoplay; clipboard-write; encrypted-media; gyroscope; picture-in-picture; web-share” referrerpolicy=”strict-origin-when-cross-origin” allowfullscreen>When it takes hold, a C. auris infection can cause various serious and even fatal illnesses in the bloodstream, the respiratory system, the central nervous system, in organs, and in the skin.
The fungus doesn’t pose much risk to the general public. Most healthy people are unlikely to pick up an infection as they’re less exposed to C. auris, and their bodies are better able to repel it.
However, for people who are already ill and in the hospital, the growing threat is a very real one. Bloodstream infections continue to be the most common, but infections in soft tissue or bone, and in cerebrospinal fluid, are increasing. The more bases there are to cover, the harder C. auris will be to control.
The pattern that’s emerging in the US is being repeated across the rest of the world, and health experts have been struggling to contain C. auris since it was first discovered in Japan in 2009. The first US cases were reported in 2016.
Several warnings have been issued about the threat posed by C. auris – including a study released almost exactly two years ago, announcing that infections had reached half of the states in the US – but as this Miami study shows, the surge is continuing.
The CDC has a lengthy list of recommendations for stopping the spread of C. auris infections, including diligent cleaning routines for surfaces and devices, and the use of single-patient rooms where possible.
“Measures to prevent the spread of C. auris rely on isolation and contact precautions,” write the researchers.
“Our findings suggest that early identification of patients colonized with C. auris and the prompt deployment of infection prevention strategies can potentially impact the incidence of bloodstream infections.”
The research has been published in the American Journal of Infection Control.